Apr 9 2018
By imitating the complex visual system of a butterfly, researchers have built a camera that offers surgeons with a traditional color image and a near-infrared image that makes fluorescently labeled cancerous cells observable even under bright surgical lighting.
The new camera is engineered to help surgeons eliminate all the cancerous cells without harming healthy tissue, making it less probable that cancer will spread and decreasing the need for many surgeries.
Instead of putting together commercially available optics and sensors to build a camera for image-guided surgery, we looked to nature’s visual systems for inspiration. The morpho butterfly, whose eyes contain nanostructures that sense multispectral information, can acquire both near-infrared and color information simultaneously.
Viktor Gruev, Research Team Leader - The University of Illinois at Urbana-Champaign
In Optica, The Optical Society's journal for high-impact research, the team demonstrates that their bio-inspired camera can spot tumors in animals and is valuable for judging the stage of breast cancer in people. The new camera offers highly sensitive fluorescence detection even under basic operating room lighting, weighs less than an AA battery, and can be produced for about $20.
During surgery, it is imperative that all the cancerous tissue is removed, and we've created an imaging platform that could help surgeons do this in any hospital around the world because it is small, compact and inexpensive. Although we’ve addressed the instrumentation side, fluorescent markers targeted for cancer and approved for use in people are needed for our technology to find widespread application. Several of these are in clinical trials now, so we should see progress in this area soon.
Viktor Gruev, Research Team Leader - The University of Illinois at Urbana-Champaign
Learning from Nature
The new camera significantly advances upon today’s cameras that are approved by the U.S. Food and Drug Administration (FDA) for seeing fluorescent markers during surgery. Many current near-infrared cameras do not possess the sensitivity to detect fluorescence markers under surgical settings, so the room lights must be dimmed to observe the fluorescence.
Another issue with present infrared imagers is that the fluorescence image is not correctly aligned all the time, or co-registered, with the tissue it arises from. This occurs because FDA-approved instruments use many optical elements, such as relay lenses and beam splitters, to divide the infrared and visible wavelengths, so that each can be conveyed to separate detectors. Minor temperature changes in the room can influence the optics in these instruments causing image misalignments that could cause a surgeon to overlook cancerous tissue while needlessly removing the healthy tissue.
“We realized that the problems of today’s infrared imagers could be mitigated by using nanostructures similar to those in the morpho butterfly,” said Missael Garcia, a post-doctoral researcher at University of Illinois at Urbana-Champaign and lead author of the paper. “Their compound eyes contain photoreceptors located next to each other such that each photoreceptor senses different wavelengths of light in a way that is intrinsically co-registered.”
The new camera uses an arrangement akin to the butterfly eye by interlacing a variety of nanoscale structures with an array of photodetectors, enabling compilation of color and near-infrared fluorescence information on a single imaging device. Combining the detector and imaging optics into one monolithic sensor keeps the device compact, low-cost, and insensitive to temperature variations.
The design exceptionally solves the sensitivity issue by permitting each pixel to take in the number of photons required to form an image. It does not take long to develop the visual-wavelength image for viewing the anatomy as the visible illumination in the laboratory is high. Conversely, because fluorescence is usually dim, it takes longer to gather an adequate number of photons to construct a considerably bright image. By altering the exposure time to allow each pixel to detect the photons it requires, a bright fluorescence image can be developed without overexposing the color image of the tissue.
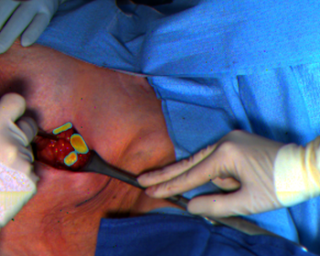 The researchers tested the ability of their infrared camera to identify lymph nodes in patients with breast cancer. Lymph nodes are one of the primary places where breast cancer spreads. The camera detects indocyanine green fluorescent dye, which accumulates passively in the lymph nodes. (Image Credit: Missael Garcia, Julie Margenthaler and Viktor Gruev)
The researchers tested the ability of their infrared camera to identify lymph nodes in patients with breast cancer. Lymph nodes are one of the primary places where breast cancer spreads. The camera detects indocyanine green fluorescent dye, which accumulates passively in the lymph nodes. (Image Credit: Missael Garcia, Julie Margenthaler and Viktor Gruev)
Preclinical and Clinical Testing
The team tried out their new instrument on a mouse model that forms spontaneous breast cancer. This means that the precise location where the cancer will develop is indefinite as is the number of cancer cells. Employing fluorescent labels that bind to cancer cells, the researchers demonstrated that their bio-inspired imager enabled tumor detection with a sensitivity and accuracy that exceeded modern infrared cameras FDA-approved for image-guided surgery.
The researchers also tested the capacity of their infrared camera to detect lymph nodes in 11 patients with breast cancer at Washington University School of Medicine in St. Louis. Since the lymph nodes are one of the main places where breast cancer spreads, surgeons check them to establish the cancer stage. The patients were injected with FDA-approved indocyanine green fluorescent dye that amasses passively in the lymph nodes and then fluorescence images from the bio-inspired imager were shown either on a screen or projected onto goggles worn by the surgeons.
We showed that under bright surgical lights, our instrument was 1000 times more sensitive to fluorescence than the imagers currently approved for infrared image-guided surgery. Because the bio-inspired imager can reveal fluorescence that is deep in the tissue, it sped up the process of lymph node identification and helped surgeons find lymph nodes that couldn’t be seen by eyesight alone.
Viktor Gruev, Research Team Leader - The University of Illinois at Urbana-Champaign
According to the researchers, the bio-inspired imager would be practical for removing several types of cancers, including prostate cancer, melanomas, and head and neck cancers. Due to its small size, it can also be combined into an endoscope to search for cancer during a colonoscopy, for instance.
“One big advantage of our instrument is its compact size,” said Garcia. “We tested our instrument in a hospital where space was tight and saw that it didn’t intrude on the surgical workflow.”
The researchers are currently developing a start-up company to commercialize their bio-inspired imager and are also collaborating with the FDA to plan a clinical trial in which the surgeons can compare clinical decisions made with the new imager with those that would be formed using FDA-approved imagers.